-
Reviewed
Key takeaways
- It’s common to have wee leakage, but there are lots of ways to manage it, including a healthy lifestyle and pelvic floor muscle exercises.
- Common symptoms of a urinary tract infection (UTI) include a burning sensation when doing a wee and needing to wee more often than usual.
- If you wake up more than once in the night to wee, you may have an overactive bladder.
- See your doctor if you are concerned about your bladder health, for example, pain when weeing.
Key takeaways
- It’s common to have wee leakage, but there are lots of ways to manage it, including a healthy lifestyle and pelvic floor muscle exercises.
- Common symptoms of a urinary tract infection (UTI) include a burning sensation when doing a wee and needing to wee more often than usual.
- If you wake up more than once in the night to wee, you may have an overactive bladder.
- See your doctor if you are concerned about your bladder health, for example, pain when weeing.
What does the bladder do?
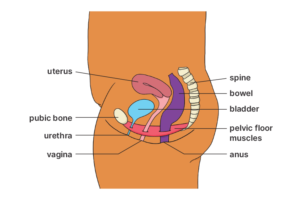
The bladder is an organ in your body that stores wee (urine) until you’re ready to go to the toilet.
It’s supported by a group of muscles called the pelvic floor. These muscles help you hold on until you reach a toilet. They also help to keep the bladder in its normal position in the pelvis. Pelvic floor muscles must relax for you to wee.
It’s common for women to experience bladder problems at different life stages, such as:
- after having a baby
- during perimenopause
- after menopause
What is the pelvic floor and why does it matter?
The pelvic floor is made up of muscles and tissues that run from your pubic bone at the front of your pelvis to your tailbone (coccyx) at the bottom of your spine. It also expands from one sitting bone to the other.
These muscles are like a supportive hammock for your bladder, bowel and uterus.
Your pelvic floor muscles are part of a muscle group known as your core. Your core muscles also include your deep abdominal and back muscles. Together with the pelvic floor muscles, they support your spine and control the pressure in your abdomen.
Your pelvic floor muscles:
- support your pelvic organs (i.e. bladder, bowel and uterus)
- help maintain control of your bladder and bowel
- improve sexual response by increasing sensation and arousal
- support your lower back and pelvis.
Learn more about pelvic floor muscles with this Continence Health Australia video.
Many factors can weaken pelvic floor muscles, for example:
- not using or exercising them
- heavy lifting
- being overweight
- pregnancy and childbirth
- chronic constipation
- chronic coughing
- perimenopause and menopause
- ageing
- high-impact exercise.
If you have weak pelvic floor muscles, you may experience:
- bladder, bowel or wind incontinence
- pelvic organ prolapse (the bladder, uterus or bowel protrudes into the vagina instead of sitting higher in the pelvis)
- difficulties emptying your bladder or bowel
- reduced sexual sensation.
Tight (overactive) pelvic floor muscles can cause health problems such as:
- constipation
- painful sex
- pelvic pain
- tension in the hip and pelvis muscles.
How to strengthen your pelvic floor muscles
In Australia, one in 3 women have a bladder control problem. Pelvic floor exercises can help you maintain strong pelvic floor muscles and prevent bladder and bowel problems throughout your life.
Pelvic floor exercises benefit people of all ages, but they are especially important:
- during pregnancy
- after childbirth
- after menopause.
Start by finding your pelvic floor muscles.
- Move into a comfortable position. A good starting point is to lie on your back (on a bed, couch or floor) with your knees bent. You can also try sitting with a straight back, leaning slightly forward.
- Squeeze the muscles around your anus, vagina and urethra quickly and strongly.
- Lift and draw these muscles up and forwards towards your belly button, then let go. Try not to squeeze your bottom. You can also imagine trying to stop weeing. Then relax as if you’re weeing again.
Once you can feel your pelvic floor muscles, you can focus on strengthening them.
It’s important to do the exercises the right way. Learn more about pelvic floor exercises on the Continence Health Australia website.
Pelvic floor strengthening exercises aren’t suitable for everyone. If you have vaginal or pelvic pain, a pelvic floor physiotherapist can help you with a program to relax these muscles.
To find a pelvic floor physiotherapist:
- go to the Find a physio webpage on the Australian Physiotherapy Association website
- choose ‘Refine your search’
- choose ‘Special interest area: Women’s, Men’s and Pelvic health’.
If you’re doing pelvic floor exercises, try to:
- exercise as often as you can (preferably daily)
- practise at a regular time (e.g. after going to the toilet).
You can also help your pelvic floor muscles by:
- lifting, holding and squeezing your muscles before sneezing, coughing, laughing or lifting
- avoiding activities that might strain your pelvic floor muscles (like heavy lifting)
- avoid constipation by eating high-fibre foods and drinking enough water
- not pushing hard when doing a poo
- drinking fluids every day (preferably water)
- maintaining a healthy weight.
If you want support or advice about strengthening your pelvic floor muscles, you can contact the National Continence Helpline.
Overactive bladder
An overactive bladder is a condition where you feel an urgent need to wee and may need to go to the toilet more often than usual, sometimes with wee leakage. This page explains the symptoms, causes, diagnosis, and treatment options, including bladder training and support from health professionals.
Urinary incontinence
Urinary incontinence is accidental wee leakage and is a common condition that can be treated, managed and sometimes cured. This page explains the types, causes, diagnosis and ways to prevent and manage urinary incontinence.
Urinary tract infections (UTIs)
A urinary tract infection (UTI) is an infection that affects the urinary system, including the bladder, urethra and kidneys. If you have a burning sensation when you wee, a frequent urge to wee and strong-smelling wee, you might have a UTI.
Bladder pain syndrome (interstitial cystitis)
Bladder pain syndrome is a condition that causes discomfort or pain in the bladder area, often with a frequent and urgent need to wee, and most commonly affects women. This page explains the symptoms, possible causes, how it’s diagnosed, and the treatment and management options available.
Our review process
This information has been reviewed by clinical experts and is based on the latest evidence.
Our content review process ensures our health information is accurate, trustworthy, current and useful.
We regularly check our information to make sure it reflects the latest clinical guidelines and key findings from large, reliable studies.
Where possible, we focus on Australian research to make our information more relevant locally.
Experts play a key role in reviewing our content. Clinicians at Jean Hailes check information for accuracy and real‑world relevance. These include GPs, gynaecologists, endocrinologists, psychologists and allied health professionals.
We also work with partner organisations, independent specialists and people with lived experience to make sure our content reflects both expert knowledge and the experiences of the community.

Want to learn more about pelvic floor exercises?
Join pelvic floor physiotherapist Janetta Webb on our podcast for simple exercises that strengthen your pelvic floor.

















