Cervical cancer develops in the cervix (the entrance to the uterus). This cancer is usually caused by the human papillomavirus (HPV). Read more about the cervical screening test, symptoms, causes and how it’s diagnosed.
Cervical cancer – screening and early detection
What is cervical cancer?
Symptoms
Causes
Diagnosis
Treatment
Prevention
When to see your doctor
Related resources
Cervical cancer develops in the cervix (the entrance to the uterus). This cancer is usually caused by the human papillomavirus (HPV). It’s important to have regular cervical screening tests to check for the presence of HPV. Regular screening prevents nine out of 10 cervical cancers. Cervical cancer vaccines are also available in Australia.
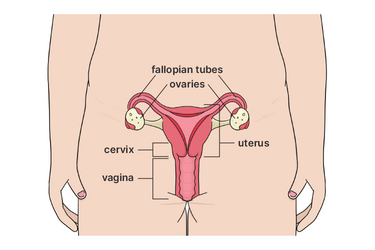
Cervical cancer develops in the cervix (the entrance to the uterus). This cancer is usually caused by the human papillomavirus (HPV).
It’s important to have regular cervical screening tests to check for the presence of HPV. Regular screening prevents nine out of 10 cervical cancers.
Cervical cancer vaccines are also available in Australia.
Learn more about cervical screening tests.
Cervical cancer is almost always caused by human papillomavirus (HPV). HPV is a common sexually transmitted infection that affects the surface cells of the genital area, including the cervix, vagina and vulva.
The best time to get immunised against HPV is before you become sexually active. Under the National Immunisation Program, a free HPV vaccine is given to people aged 12 to 13 at school.
If you have been vaccinated for HPV, it’s still important to get regular cervical screening tests. While the HPV vaccine is highly effective, it doesn’t prevent all HPV infections.
See your doctor for more information about the HPV vaccine.
Cervical cancer develops in the cervix (the entrance to the uterus). Cervical cells can change over time and they may become cancerous.
Cervical cancer is the 13th most diagnosed cancer in women in Australia.
There are two types of cervical cancer:
Some cervical cancers have both squamous and glandular cells.
Cervical cancer is more common in people over 30, although it can occur at any age. In Australia, a female has a one in 180 risk of being diagnosed with cervical cancer by the age of 85.
Symptoms of cervical cancer may not be obvious, especially in the early stages. But symptoms may include:
Symptoms may also include:
Symptoms of advanced cervical cancer may include:
Many of these symptoms may be related to other conditions, but if you’re worried, talk to your doctor.
Cervical cancer is almost always caused by human papillomavirus (HPV).
HPV is a common sexually transmitted infection that affects the surface cells of the genital area, including the cervix, vagina and vulva. It can also cause visible warts.
HPV is very common. About 80% of women will have the virus at some point in their lives, but many don’t know they've been exposed to the infection.
Most women with the infection don’t develop cervical cancer. Only certain types of HPV cause cancer.
Cervical cancer usually develops many years after the HPV infection occurs.
There are some other risk factors associated with cervical cancer. For example:
Like many cancers, early diagnosis and detection lead to the best treatment outcomes.
A cervical screening test will check for HPV. If HPV is not detected, you can wait five years until your next test.
If you have an abnormal test result, you may need further tests, such as a second cervical screening test or a colposcopy. A colposcopy is when an instrument is used to look closely at your cervix and check for abnormal cells, and tissue samples (biopsy) are taken for testing.
If abnormal or cancerous cells are detected, your doctor will refer you to a cancer specialist for treatment.
If precancerous cells are detected, treatment may include:
Treatment for cervical cancer depends on the size and type of cancer, but it may include:
Cancer treatment, such as chemotherapy and radiotherapy, can cause menopause. Learn more about menopause due to cancer treatment.
You can lower your risk of cervical cancer by:
See your doctor for regular cervical screening tests, and to get the HPV vaccine if you haven’t already had it. It’s important to see your doctor if you notice any symptoms of cervical cancer. In most cases, early detection and diagnosis lead to good outcomes.
This content has been reviewed by a group of medical subject matter experts, in accordance with Jean Hailes policy.
© Jean Hailes Foundation. All rights reserved.