A hysterectomy is an operation to remove your uterus. There are many reasons for having a hysterectomy. For example, certain health conditions and diseases, persistent pelvic pain and cancer. If you have a hysterectomy, you will not be able to carry a pregnancy in the future.
Learn more about how a hysterectomy is performed, and the risks and benefits of this procedure.
What is a hysterectomy?
Reasons for having a hysterectomy
Do you need a doctor’s referral?
How is a hysterectomy performed?
Risks of having a hysterectomy
Outcomes
Related resources
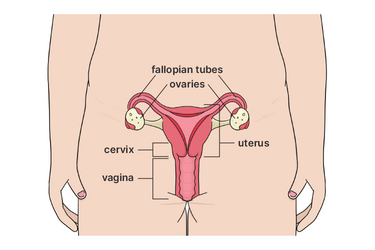
A hysterectomy is an operation to remove your uterus. There are two types of hysterectomies.
Removal of your uterus and cervix. Often your fallopian tubes are removed at the same time, as this reduces the chance of ovarian cancer by 60%.
Removal of your uterus, leaving the cervix in place. Often your fallopian tubes are removed at the same time. This procedure may be done to help manage pelvic organ prolapse.
Your doctor will usually recommend your fallopian tubes are removed and your ovaries are left behind as this may benefit your heart and bone health up until the age of 64 – long after menopause.
Your doctor might recommend you have a hysterectomy for different reasons. For example, if you have:
A hysterectomy is an irreversible procedure. There are many things to consider such as your plans to have children and the severity of your symptoms. You can ask your doctor about different options and the benefits and risks of each. If you are still unsure, you can talk to a specialist or get a second opinion.
You will need a doctor’s referral for a gynaecologist who can perform the hysterectomy.
There are different ways to perform a hysterectomy, depending on the reason for the procedure, your medical history and general health.
For example:
Hysterectomies are usually performed under general anaesthetic.
As with any operation, there are some risks associated with having a hysterectomy. For example, you might:
Compared to abdominal hysterectomy, vaginal and laparoscopic hysterectomies have lower risks of blood loss and infection.
Your specialist will explain the risks in more detail.
Studies suggest that many women have improved symptoms, mood and quality of life after recovering from a hysterectomy.
It may take up to four weeks to recover fully after vaginal or laparoscopic hysterectomy and up to six weeks after abdominal hysterectomy. But it can take longer for some women, depending on their individual situation (e.g. complications during surgery or emotional adjustment).
Visit the Royal Australian and New Zealand College of Obstetricians and Gynaecologists (RANZCOG) website to learn more about recovering from a hysterectomy.
This content has been reviewed by a group of medical subject matter experts, in accordance with Jean Hailes policy.
© Jean Hailes Foundation. All rights reserved.